
The sleep disturbance must occur despite adequate opportunity for sleep in a safe, dark environment. This daytime dysfunction can manifest in a wide range of ways, including fatigue, malaise impairment in attention, concentration or memory impaired social, family, occupational or academic performance mood disturbance, irritability, sleepiness, hyperactivity, impulsivity, aggression, reduced motivation, proneness for errors, and concerns about or dissatisfaction with sleep 2. The clinical diagnosis of insomnia is based on the complaint of trouble falling asleep, trouble staying asleep, or early morning awakening, and resultant daytime dysfunction 1, 2.
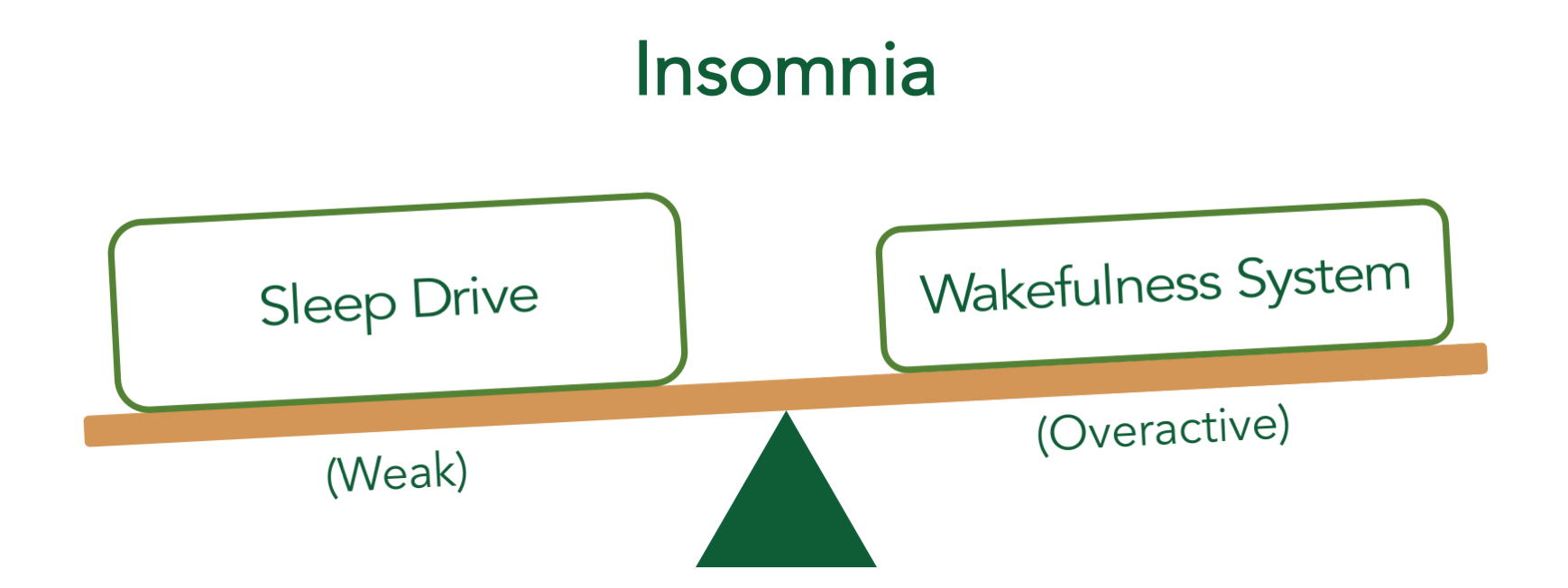
This paper reviews the state of the art for optimally diagnosing and treating insomnia based on the available research evidence. The public health impact of this condition in terms of prevalence, morbidity and consequences on health and quality of life highlights the need to effectively diagnose and treat it in clinical practice. These include non‐medication therapies as well as medication options 25, 26, 27, 28. On this basis, as well as due to the fact that insomnia is associated with impairments in quality of life and an increased risk for accidents and falls, it is recommended that treatment be targeted specifically to addressing insomnia whenever it is present, including when it occurs along with physical or psychiatric conditions 24, 25.įor those who meet the diagnostic criteria for insomnia, a number of empirically supported treatments are available. In fact, insomnia is a risk factor for major depression, anxiety disorders, substance use disorders, suicidality, hypertension and diabetes 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23. Although it had long been believed that, when this was the case, insomnia was a symptom of those conditions, the available evidence suggests that the relationship between such conditions and insomnia is complex and sometimes bidirectional 7, 8, 9, 10. In the vast majority of cases, insomnia co‐occurs with psychiatric or physical conditions. It is a common condition, with an approximate general population point prevalence of 10% 3, 4, 5, 6. Insomnia is defined as a complaint of difficulty falling or staying asleep which is associated with significant distress or impairment in daytime function and occurs despite an adequate opportunity for sleep 1, 2. We review this evidence base and highlight areas where more studies are needed, with the aim of providing a resource for improving the clinical management of the many patients with insomnia. These interventions can form the basis for systematic, evidence‐based treatment of insomnia in clinical practice. However, there are an array of interventions which have been demonstrated to have therapeutic effects in insomnia in trials with the above features, and whose risk/benefit profiles have been well characterized. A review of the available research indicates that rigorous double‐blind, randomized, controlled trials are lacking for some of the most commonly administered insomnia therapies. These options include both non‐medication treatments, most notably cognitive behavioral therapy for insomnia, and a variety of pharmacologic therapies such as benzodiazepines, “z‐drugs”, melatonin receptor agonists, selective histamine H1 antagonists, orexin antagonists, antidepressants, antipsychotics, anticonvulsants, and non‐selective antihistamines. To this end, this paper reviews critical aspects of the assessment of insomnia and the available treatment options. As such, it is important that effective treatment is provided in clinical practice.
It is a common condition associated with marked impairment in function and quality of life, psychiatric and physical morbidity, and accidents. Insomnia poses significant challenges to public health.


 0 kommentar(er)
0 kommentar(er)
